What are Digestive Organs?
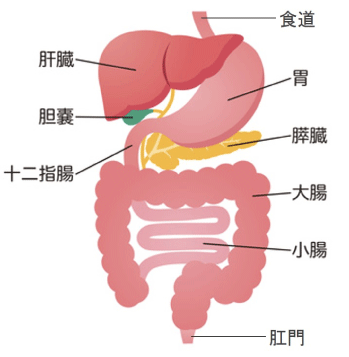
The digestive organs can be broadly categorized into:
- 01. Digestive tract (esophagus, stomach, duodenum, small intestine, large intestine, rectum)
- 02. Liver
- 03. Pancreas
- 04. Gallbladder and bile ducts
These form the digestive system.
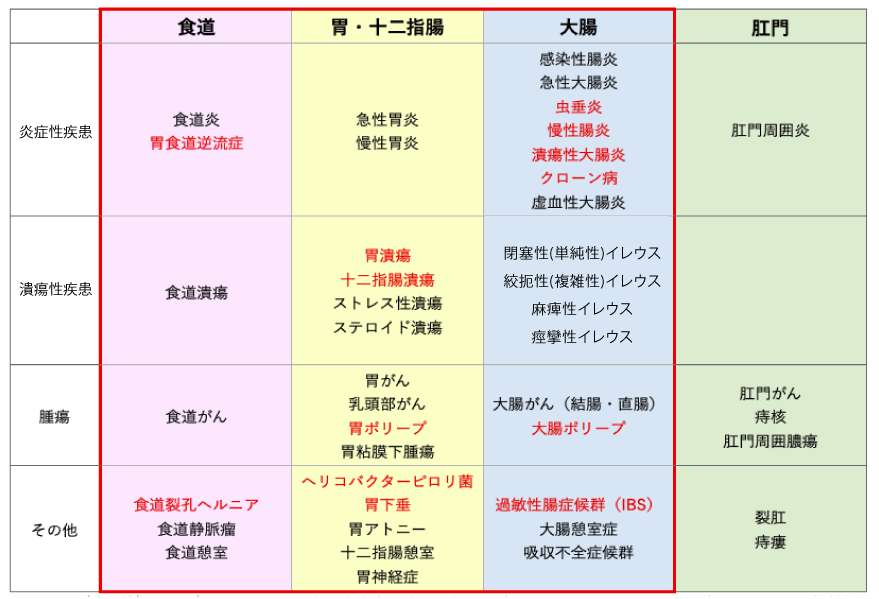
Representative Diseases
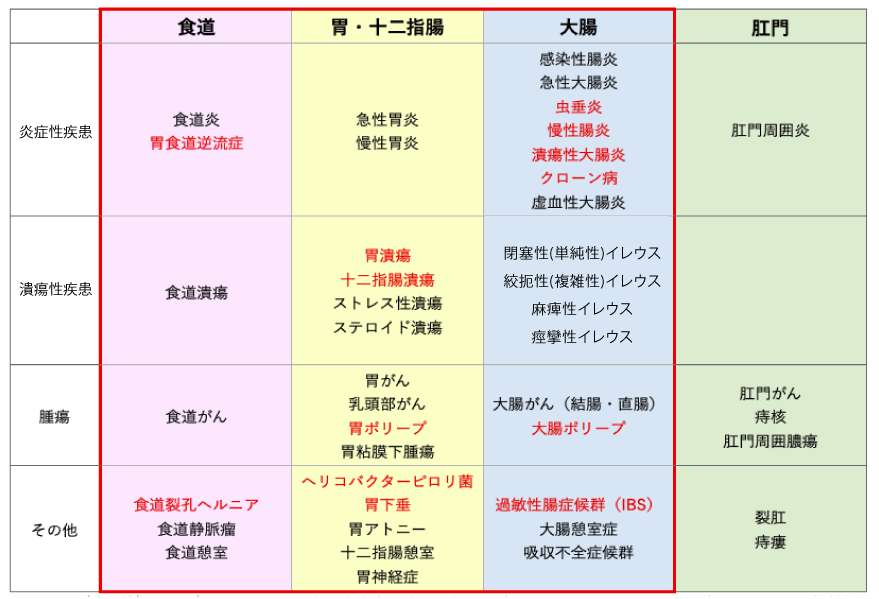
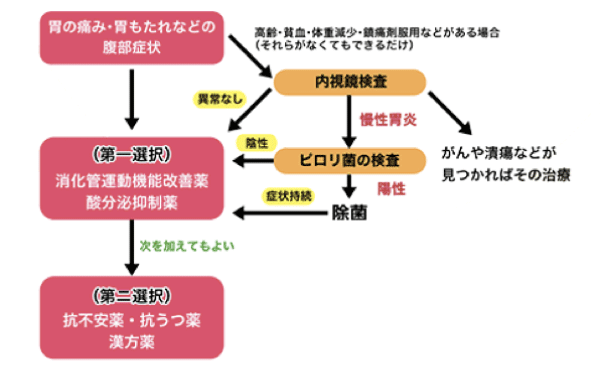
In this Gastrointestinal (Digestive Tract) Care Program, we address not only the diseases highlighted in the red box in the chart but also Functional Dyspepsia (FD), which presents chronic discomfort such as epigastric pain or bloating, even without any identifiable abnormalities causing the symptoms.
What is Functional Dyspepsia (FD)?
Definition of Functional Dyspepsia
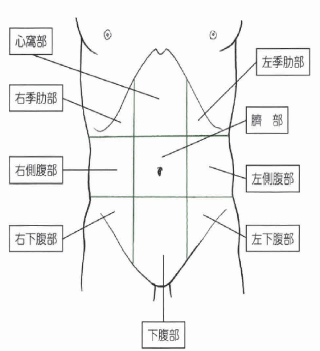
A disease characterized by chronic abdominal symptoms centered around the epigastric region, such as epigastric pain and bloating, despite the absence of any underlying organic, systemic, or metabolic disorders.
The term “dyspepsia” originates from Greek, meaning “indigestion.”
Previously, such symptoms were commonly diagnosed as “chronic gastritis,” which refers to “inflammation of the stomach” (most often caused by Helicobacter pylori). However, it has become clear that the presence of inflammation is not directly correlated with symptoms.
As a result, since around the 1990s, the concept of Functional Dyspepsia (FD) has been proposed by the American Gastroenterological Association.
Currently, the prevalence rate of Functional Dyspepsia is reported to be as high as 15%. While it is not a life-threatening condition, it affects quality of life (QOL) and therefore requires appropriate treatment.
Causes
In some cases, there is only one cause, while in others, multiple factors contribute to the symptoms.
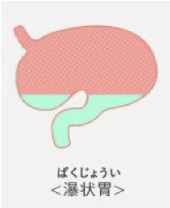
- When gastric and duodenal motility is impaired: This includes abnormalities in gastric emptying and adaptive relaxation.
- When hypersensitivity of the gastric and duodenal regions occurs: Symptoms arise even with mild gastric distension compared to healthy individuals.
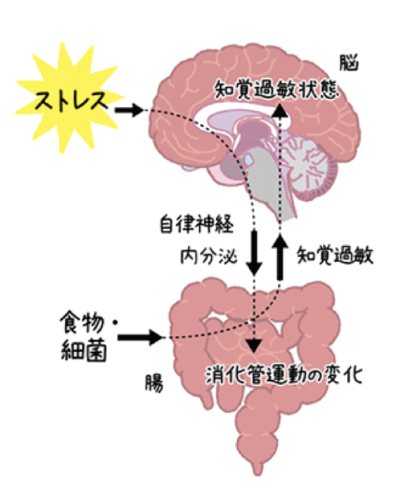
- When psychological factors (especially anxiety or a history of abuse) are present: The brain and gut are closely interconnected.
Examination and Diagnosis
We perform endoscopic gastric examinations to rule out diseases such as stomach cancer, gastric ulcers, and duodenal ulcers, as well as tests for Helicobacter pylori infection. If necessary, blood tests, ultrasound examinations, and abdominal CT scans may also be performed.
Diagnostic Criteria
・Presence of chronic stomach pain or bloating as self-reported symptoms
※Specifically, symptoms such as post-meal bloating, early satiety, epigastric pain, and epigastric burning sensation
・If diseases such as stomach cancer or gastric ulcers are not found in endoscopic examination or other tests
General Treatment
There are mainly two possible causes for FD (Functional Dyspepsia) symptoms.
・When abnormalities in the stomach function are felt as symptoms
Stimulants that cause abnormalities typically include stomach movement and stomach acid. If the series of movements that send food from the stomach to the duodenum does not proceed smoothly, bloating and pain symptoms can occur. For improvement, gastrointestinal motility improving medications are used. In addition, stomach acid secretion may cause pain, or excessive stomach acid flowing into the duodenum may cause nausea. To suppress stomach acid secretion, acid secretion inhibitors are used.
・When symptoms appear due to heightened sensitivity to normal stomach function
This occurs when the body becomes overly sensitive to various stimuli. It is difficult to control the overly sensitive brain state, but certain anti-anxiety medications and antidepressants have been shown to improve FD symptoms. Moreover, herbal medicines have been suggested to improve stomach movement or increase appetite, which may improve FD symptoms, but there is not enough evidence to fully support this yet.
In consultation with the patient and physician, we may try different medications, and sometimes use a combination of medications with different effects for treatment. Under the guidance of a trusted physician, it is essential to take the correct medications along with improving lifestyle and eating habits.
Recovery Rate and Associated Diseases
Unfortunately, methods for preventing recurrence and identifying individuals who are likely to relapse are not yet clearly known. However, it is said that about 20% of patients experience a relapse within a few months after symptoms have disappeared following treatment.
Psychosocial factors are believed to be involved, and mood disorders such as anxiety, depression, and neurotic disorders often accompany the condition. It is reported that 25-50% of individuals may also have gastroesophageal reflux disease, irritable bowel syndrome, or chronic constipation. In some cases, diseases related to the gallbladder or pancreas may be hidden.
Irritable Bowel Syndrome (IBS)
Irritable Bowel Syndrome (IBS)
This disease is most suspected when abdominal pain and discomfort, along with related abnormal bowel movements such as constipation or diarrhea (changes in frequency and consistency), continue for several months. The absence of organic diseases such as tumors or inflammation in the large intestine is a prerequisite for this diagnosis.
It is estimated that about 10% of the Japanese population suffers from this condition, and many individuals are affected. It is more common in women, and its prevalence decreases with age. While it is not a life-threatening condition, it can interfere with daily life due to symptoms such as abdominal pain, constipation, diarrhea, and anxiety.
Causes
The intestines not only digest and absorb but also excrete waste as stool. Therefore, contraction movements in the intestines and sensory functions that detect changes are necessary for moving food toward the anus. This process is controlled by the exchange of information between the brain and the intestines. When in a state of anxiety due to stress, the contraction movements become excessive, and the sensitivity of the sensory functions increases. This heightened state is a characteristic of IBS. Stress strengthens signals from the brain to the intestines, altering gastrointestinal motility through autonomic nerves and the endocrine system.
The exact cause of IBS is not well understood, but it is known that IBS is more likely to develop after infection with bacterial or viral gastroenteritis.
Examination and Diagnosis
Since IBS is characterized by abdominal symptoms and abnormal bowel movements, it may be diagnosed through questioning alone without the need for special tests. However, to confirm that no serious organic diseases such as colon cancer or inflammatory bowel disease are present, or in severe cases or when symptoms do not improve despite treatment, additional tests such as blood tests, abdominal ultrasound, abdominal CT scans, stool occult blood tests, colonoscopy, and barium enema may be performed.
Diagnostic Criteria (Rome III Criteria)
Within the past three months, abdominal pain or discomfort has occurred on three or more days per month, and two or more of the following characteristics are present:
1) Symptoms improve after bowel movements
2) Frequency of bowel movements changes (increased or decreased)
3) The appearance of stools changes along with the symptoms (becoming softer or harder)
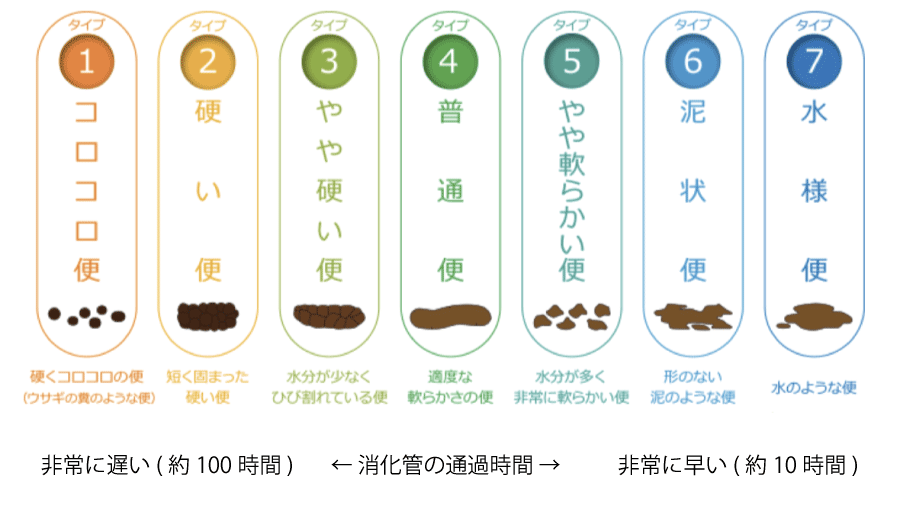
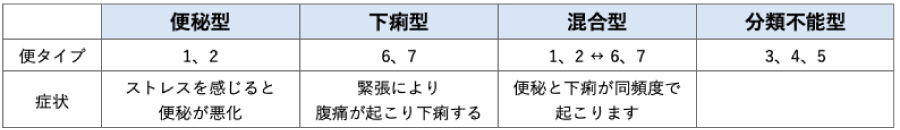
Type Classification
The Bristol Stool Scale, a rating scale, is used to classify the stool shape and frequency into four types.
General Treatment
・First, lifestyle improvements are recommended.
Avoid overeating, excessive drinking, and maintain a balanced diet with regular meals. Avoid accumulating stress, and ensure adequate sleep and rest. Limit the intake of stimulants, high-fat foods, and alcohol.
・If symptoms do not improve after lifestyle changes, pharmacological treatment may be used.
> Initially, gastrointestinal motility regulators, probiotics (such as bifidobacteria and lactobacilli), and medications that adjust the water balance in stools may be used. These medications are used for both diarrhea-dominant and constipation-dominant patients.
> For diarrhea type patients, serotonin 3 receptor antagonists (5-HT3 antagonists) may be used to improve abnormal intestinal movement.
> For constipation type patients, medications that soften stool may be used.
Antidiarrheal medications for diarrhea, anticholinergic drugs for abdominal pain, and laxatives for constipation may also be used as adjunctive or as-needed treatments.
・Non-pharmacological treatments include diet therapy and exercise therapy.
Foods that are likely to induce abdominal pain or changes in bowel movements include carbohydrates, high-fat foods, coffee, alcohol, and spicy foods. If there are specific trigger foods, it is advised to avoid them. Fermented foods like yogurt are effective in alleviating symptoms. Additionally, fiber-rich foods are effective for constipation-dominant IBS. Moderate exercise is also expected to reduce symptoms. Aim to incorporate manageable exercise into your routine.
・If pharmacological therapy does not sufficiently alleviate IBS symptoms, psychotherapy may be effective.
When stress or psychological factors are strongly related, combined therapy with psychological therapy and medication may be used.
Precautions
Abdominal pain and bowel movement abnormalities tend to improve with age, and the risk of disease is lower. However, it is important to avoid long-term use of antidiarrheal medications or laxatives and ensure that lifestyle improvements are consistently followed to prevent recurrence.